Introduction
Miscarriage, the loss of pregnancy before 20 weeks, can be an emotionally devastating experience. This is particularly common in the first trimester when the body is still adjusting to pregnancy, and the developing embryo is most vulnerable. Understanding the common reasons for miscarriage in the first trimester can be empowering for those trying to conceive or those who have experienced a loss. While the causes are often out of anyone’s control, awareness can help women and their partners seek the right medical guidance and emotional support.
In this comprehensive blog post, we’ll explore the leading causes of early miscarriage, symptoms to watch for, and what can be done to reduce the risk in future pregnancies. Let’s start by understanding what a miscarriage is and how common it is in the first trimester.
What is a Miscarriage?
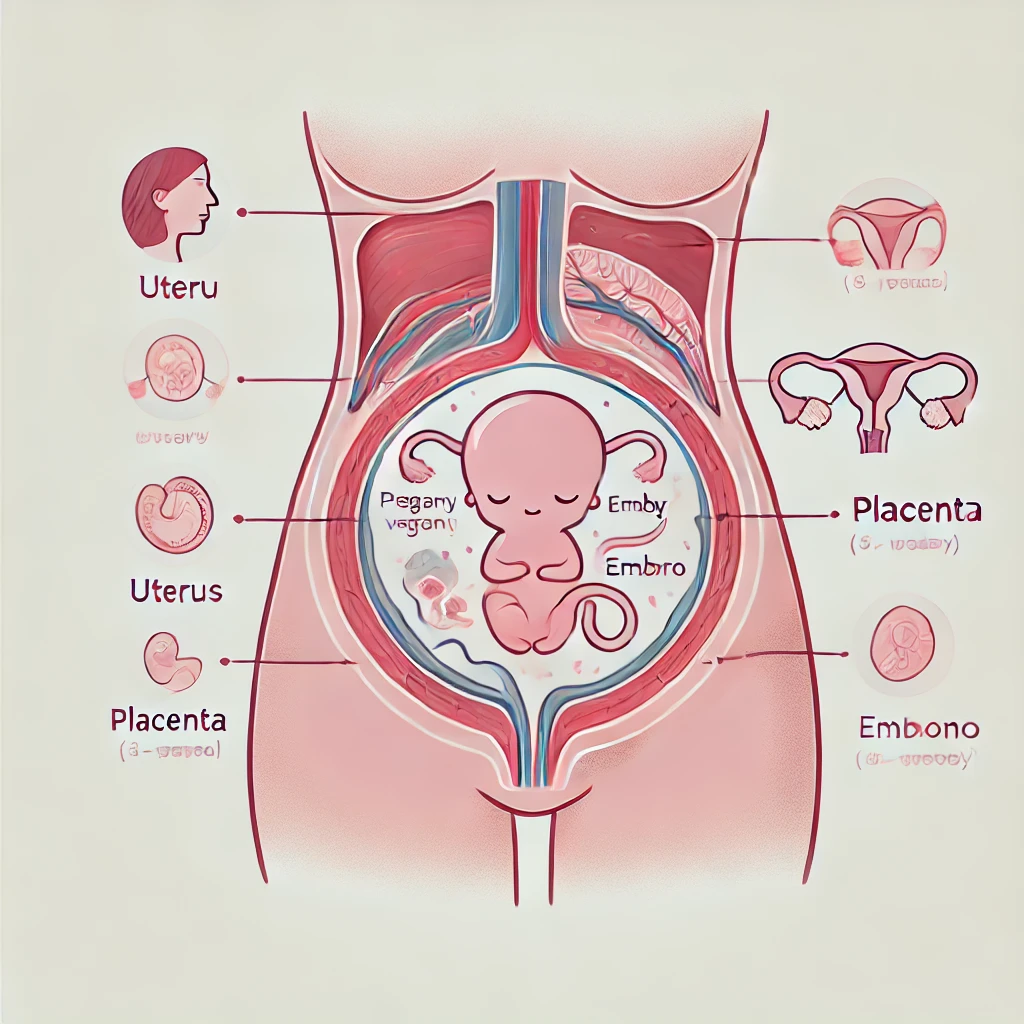
A miscarriage, also referred to as spontaneous abortion, is the loss of a pregnancy before the 20th week. This can happen for a variety of reasons, and while it’s a natural part of reproductive health, it often leaves emotional scars for those affected. Understanding the basics of miscarriage helps to demystify some of the pain and confusion surrounding it.
Types of Miscarriages
There are different types of miscarriages, and knowing the type can sometimes provide clues about the underlying cause:
- Chemical Pregnancy: This occurs when an embryo implants in the uterus but doesn’t develop. Many women might not even know they were pregnant since this often happens around the time of their expected period.
- Missed Miscarriage: In this case, the embryo has died, but the body hasn’t recognized the loss yet, meaning there are no immediate symptoms like bleeding or cramping.
- Complete Miscarriage: This happens when all pregnancy tissues are expelled from the uterus. Bleeding and cramping are common symptoms.

How Common are Miscarriages?
Miscarriage is much more common than many people realize. It is estimated that 10-20% of known pregnancies end in miscarriage, but this number could be higher because many early miscarriages occur before a woman even realizes she is pregnant.
The majority of miscarriages (around 80%) happen during the first trimester, often before the 12th week of pregnancy. The first trimester is a critical period when the embryo is rapidly growing and developing, but it’s also when things can most easily go wrong.
Most Common Reasons for Miscarriage in First Trimester
Miscarriages are rarely caused by something the mother did or didn’t do. Instead, they are often linked to factors beyond anyone’s control, particularly when they occur in the early stages of pregnancy. Below are the most common reasons for miscarriage in the first trimester:
1. Chromosomal Abnormalities
Chromosomal abnormalities are by far the most common cause of first-trimester miscarriage. In fact, it is estimated that 50-70% of first-trimester miscarriages are the result of problems with the chromosomes.
Chromosomes carry the genetic material from both the mother and the father. Normally, a baby has 46 chromosomes, 23 from each parent. However, sometimes there are errors during the process of fertilization that can result in missing or extra chromosomes. These chromosomal abnormalities can prevent the embryo from developing normally, leading to miscarriage.
Common Chromosomal Abnormalities Include:
- Trisomy: When there is an extra chromosome. The most well-known example is Down syndrome (Trisomy 21), but others like Trisomy 18 and Trisomy 13 are often fatal.
- Monosomy: When one of the pairs of chromosomes is missing. An example is Turner syndrome, where only one X chromosome is present.
While chromosomal abnormalities are usually random, the risk increases as a woman gets older. This is why women over 35 have a higher chance of miscarriage due to chromosomal issues.
Case Study:
A 2019 study published in Obstetrics & Gynecology found that 70% of miscarriages in women over 35 were linked to chromosomal abnormalities, emphasizing the role of age and genetic factors in early pregnancy loss.
Read more: Top Tips for a Healthy 1st Trimester
When Does the First Trimester End? A Complete Guide to Early Pregnancy
2. Maternal Health Conditions
A mother’s overall health can significantly impact the health of her pregnancy. Several pre-existing health conditions can increase the risk of miscarriage during the first trimester.
- Hormonal Imbalances: Conditions like Polycystic Ovary Syndrome (PCOS) or problems with the thyroid can cause hormonal fluctuations that disrupt the early stages of pregnancy. For instance, low levels of progesterone (a hormone crucial for maintaining pregnancy) can make it difficult for the embryo to implant or grow properly.
- Uncontrolled Diabetes: When blood sugar levels are poorly managed, it can create an unhealthy environment for the developing fetus. High blood sugar levels can damage the blood vessels in the placenta, leading to early pregnancy loss. Women with Type 1 or Type 2 diabetes should work closely with their healthcare provider to keep their blood sugar levels stable during pregnancy.
- Autoimmune Disorders: Conditions like lupus or antiphospholipid syndrome (APS) can cause the immune system to attack the developing embryo. APS, in particular, causes blood clots to form, which can block the blood flow to the fetus, resulting in miscarriage.
List of Maternal Health Conditions That Can Lead to Miscarriage:
- Hypothyroidism or hyperthyroidism
- Polycystic Ovary Syndrome (PCOS)
- Type 1 or Type 2 diabetes
- Autoimmune disorders like lupus or APS
Proactive management of these conditions before and during pregnancy can help reduce the risk of miscarriage. For example, maintaining proper thyroid levels and controlling blood sugar can significantly improve pregnancy outcomes.
3. Age of the Mother
As women age, the quality and quantity of their eggs decline. This is one of the primary reasons why miscarriage rates increase with age. For women in their 20s, the chance of miscarriage is approximately 10-15% per pregnancy, while for women over 35, that risk rises to 20-35%. By age 40, the risk can be as high as 40-50%.
The link between age and miscarriage largely comes down to egg quality. As a woman ages, her eggs are more likely to have chromosomal abnormalities, which, as mentioned earlier, are the most common cause of miscarriage in the first trimester.
4. Lifestyle Factors
While many miscarriages are the result of genetic or biological factors, certain lifestyle choices can also play a role in increasing the risk of miscarriage, especially in the early stages of pregnancy.
- Smoking: Cigarette smoke contains harmful chemicals like nicotine and carbon monoxide that reduce the amount of oxygen available to the fetus. Studies have shown that women who smoke are at a 25% higher risk of miscarriage compared to non-smokers.
- Alcohol: Excessive alcohol consumption during pregnancy can interfere with fetal development. Research suggests that even moderate drinking increases the risk of miscarriage, especially in the first trimester.
- Substance Abuse: Illicit drugs, such as cocaine or methamphetamine, can cause placental problems, leading to miscarriage. Even certain prescription medications, if not monitored closely, can pose risks during pregnancy.
- Poor Nutrition: Nutrient deficiencies, especially in folic acid, have been linked to birth defects and miscarriage. A balanced diet rich in essential vitamins and minerals is crucial during early pregnancy. Folic acid supplements are often recommended to reduce the risk of miscarriage and neural tube defects.
Key Lifestyle Factors that Can Increase Miscarriage Risk:
- Smoking
- Alcohol consumption
- Drug use
- Poor diet or nutritional deficiencies
By making healthier lifestyle choices, women can reduce their risk of miscarriage and promote a healthy pregnancy.
5. Infections
Infections during pregnancy, especially in the first trimester, can pose a significant risk to both the mother and the developing fetus. While many infections may seem mild to the mother, they can severely affect the embryo’s growth and lead to miscarriage. Some infections cause inflammation or directly interfere with the placenta, which nourishes the fetus, while others can lead to fever or other symptoms that impact early pregnancy.
Common Infections That Can Cause Miscarriage
- Rubella (German measles): Rubella is a viral infection that can have serious consequences if contracted during pregnancy. It is known to cause miscarriage or stillbirth, especially if the mother is infected during the first trimester. Thankfully, the rubella vaccine has significantly reduced its prevalence, but it’s still important for women to ensure they are vaccinated before becoming pregnant.
- Toxoplasmosis: This infection is caused by a parasite often found in undercooked meat or contaminated water. It can also be contracted by coming into contact with cat feces. While it may not cause noticeable symptoms in the mother, toxoplasmosis can lead to severe complications in early pregnancy, including miscarriage.
- Listeria: Found in contaminated food, such as unpasteurized dairy products and undercooked meats, listeria can cause an infection that leads to miscarriage or stillbirth. Pregnant women are advised to avoid high-risk foods to minimize the chance of contracting this infection.
- Sexually Transmitted Infections (STIs): Certain STIs, such as chlamydia, gonorrhea, and syphilis, can increase the risk of miscarriage if left untreated. These infections can cause inflammation in the reproductive organs or pass the infection to the developing fetus, leading to complications or pregnancy loss.
- Cytomegalovirus (CMV): CMV is a common virus that most people contract at some point in their lives. While it’s usually harmless, contracting it for the first time during pregnancy can cause severe developmental issues in the fetus, potentially leading to miscarriage.
How Infections Affect Pregnancy
Infections can cause miscarriage in a few different ways. Some infections lead to fever, which can disrupt the developing embryo’s environment. Others can cause inflammation or an immune response, which may make it difficult for the pregnancy to progress. In certain cases, the infection can damage the placenta, which is crucial for nutrient and oxygen exchange between the mother and fetus. Without proper placental function, the embryo cannot survive.
Preventing Infections During Pregnancy
- Vaccinations: Ensure you are up-to-date on all vaccinations, including rubella and the flu shot, before trying to conceive.
- Food Safety: Avoid high-risk foods like raw or undercooked meats, unpasteurized dairy products, and cold deli meats.
- Hygiene Practices: Wash hands frequently, especially after handling raw meat, gardening, or cleaning a litter box.
- STI Screening: Regular screenings for sexually transmitted infections before and during pregnancy can prevent complications.
By being proactive about preventing infections, you can reduce the risk of complications during early pregnancy and lower the likelihood of miscarriage.
6. Physical Trauma
Physical trauma is a less common but still significant cause of miscarriage in the first trimester. The body is resilient, and minor bumps or falls usually do not lead to pregnancy loss. However, severe trauma, particularly to the abdomen, can disrupt the pregnancy.
Read More: First Trimester Tips: What to Expect in the First 13 Weeks of Pregnancy
Types of Trauma That Can Lead to Miscarriage
- Car Accidents: A high-impact car crash can cause injury to the uterus or placenta, leading to miscarriage. Even if the trauma is not directly to the abdomen, the sudden force can affect the pregnancy.
- Serious Falls: While most small falls or slips will not harm a pregnancy, a significant fall with a strong impact on the abdominal area can pose a risk.
- Violence or Assault: Sadly, physical violence or assault can cause miscarriage, especially if there is direct injury to the abdomen.
Myths About Trauma and Miscarriage
Many myths exist around physical activity and pregnancy, but it’s important to understand what is safe and what isn’t. Common misconceptions include:
- Exercise Causes Miscarriage: Regular exercise is actually beneficial during pregnancy and is generally encouraged. However, high-impact activities, contact sports, or exercises that pose a risk of falling should be avoided.
- Sex Can Cause Miscarriage: In healthy pregnancies, sex does not cause miscarriage. However, if a woman has a high-risk pregnancy or certain complications, her doctor may advise caution.
What to Do If You Experience Trauma During Pregnancy
If you experience any form of physical trauma while pregnant, it’s important to seek medical attention, even if you feel fine. Your healthcare provider can perform tests such as ultrasounds or fetal heart monitoring to ensure the pregnancy is still progressing normally.
7. Uterine Abnormalities and Cervical Insufficiency
Structural issues with the uterus or cervix can also contribute to first-trimester miscarriages. These issues may make it difficult for the embryo to implant properly or for the pregnancy to continue as the baby grows.
Common Uterine Abnormalities
- Fibroids: These are benign growths in the uterus. Depending on their size and location, fibroids can interfere with implantation or restrict space for the growing fetus, leading to miscarriage.
- Septate Uterus: This is a congenital condition where the uterus is divided by a wall of tissue, called a septum. If the embryo implants on the septum, it may not receive enough blood flow to sustain pregnancy, resulting in early loss.
- Bicornuate Uterus: In this condition, the uterus is heart-shaped rather than pear-shaped, which can limit the space available for the baby to grow. This structural abnormality is associated with higher rates of miscarriage and preterm birth.
Cervical Insufficiency
Cervical insufficiency occurs when the cervix begins to open or shorten too early in pregnancy, typically after the first trimester. However, in some cases, it can cause miscarriage early on. Normally, the cervix stays closed during pregnancy until labor begins, but if it opens too soon, the risk of miscarriage or preterm labor increases.
Treatments and Solutions
- Surgery: In some cases, surgery may be required to correct uterine abnormalities. For example, a septate uterus can often be repaired with a minimally invasive procedure called a hysteroscopic resection.
- Cervical Cerclage: If a woman is diagnosed with cervical insufficiency, her doctor may recommend a procedure called cerclage, where the cervix is sewn closed to prevent it from opening too early.
While structural abnormalities of the uterus or cervix can contribute to miscarriage, many women with these conditions can still have healthy pregnancies, especially with appropriate medical intervention.
8. Environmental and Occupational Hazards
Another often overlooked cause of first-trimester miscarriages is exposure to certain environmental or occupational hazards. While most daily activities are safe, some substances and environmental conditions can pose serious risks to a developing fetus, especially during the early stages of pregnancy when the embryo is most vulnerable.
Common Environmental Hazards
- Exposure to Chemicals: Prolonged exposure to certain chemicals can increase the risk of miscarriage. Women working in environments where they are exposed to pesticides, solvents, or heavy metals should take extra precautions. Pesticides used in agriculture, as well as certain industrial solvents, have been linked to pregnancy complications and early miscarriage.
- Radiation Exposure: High levels of radiation, such as that experienced during radiation therapy or in certain industrial environments, can be harmful to both the mother and the fetus. Even X-rays should be avoided or minimized during pregnancy unless absolutely necessary.
- Air Pollution: Studies have shown a link between high levels of air pollution and an increased risk of miscarriage. In particular, exposure to high levels of particulate matter (PM2.5) and carbon monoxide can affect pregnancy outcomes, especially in urban areas with poor air quality.
- Household Chemicals: Some everyday household products, such as certain cleaning agents, paint thinners, and nail polish removers, contain chemicals that could be harmful during pregnancy if inhaled or absorbed in large amounts. Pregnant women should ensure proper ventilation when using these products and consider switching to more natural, chemical-free alternatives.
Occupational Hazards
Women in certain professions may face additional risks due to the nature of their work. Jobs that involve heavy lifting, standing for long periods, or exposure to harmful substances can increase the likelihood of a miscarriage in the first trimester.
High-Risk Jobs Include:
- Healthcare Workers: Exposure to infectious diseases, radiation, and certain chemicals can be hazardous during pregnancy. Nurses, radiologists, and lab technicians are at higher risk.
- Factory Workers: Women who work in factories where they are exposed to chemicals, such as those used in manufacturing or cleaning, may be at higher risk of miscarriage.
- Agricultural Workers: Pesticides used in farming can be harmful if pregnant women are exposed to them regularly. Wearing protective gear and minimizing exposure is essential.
Protecting Yourself from Environmental and Occupational Risks
- Avoiding Harmful Chemicals: Whenever possible, avoid exposure to known harmful chemicals, both at home and at work. If your job requires exposure to these substances, work with your employer to find ways to limit contact during pregnancy.
- Personal Protective Equipment (PPE): If you cannot avoid exposure, ensure that you are using proper PPE, such as gloves, masks, or respirators, to minimize risk.
- Regular Monitoring: If you work in a high-risk environment, frequent check-ins with your healthcare provider can help ensure that your pregnancy is progressing normally. You may also need additional monitoring or precautions based on your job or living environment.
By being aware of environmental and occupational hazards and taking appropriate steps to minimize exposure, women can help protect themselves and their pregnancies.

9. Genetic Factors and Inherited Conditions
Sometimes, miscarriages in the first trimester are the result of underlying genetic factors passed down from one or both parents. While chromosomal abnormalities are a common cause, as mentioned earlier, other genetic issues can also interfere with pregnancy, leading to early loss.
Inherited Genetic Disorders
Some genetic disorders that are passed from parent to child can increase the risk of miscarriage. These disorders often affect how the embryo develops or how the body sustains a pregnancy.
Examples of Genetic Factors Include:
- Balanced Translocation: In some cases, one or both parents may have a condition called balanced translocation, where a portion of one chromosome has transferred to another chromosome. While the parent may not show any symptoms, the embryo may inherit an unbalanced set of chromosomes, leading to miscarriage.
- Single Gene Mutations: Inherited conditions, such as cystic fibrosis or sickle cell disease, can sometimes lead to complications during pregnancy. Although these conditions are usually detected before conception, they may contribute to recurrent miscarriages if they are not identified and managed early on.
- Thrombophilia: This is a group of conditions where the blood has an increased tendency to form clots. Certain types of thrombophilia, such as Factor V Leiden or prothrombin gene mutation, can interfere with the blood supply to the developing fetus, leading to miscarriage.
Diagnosing Genetic Issues
When a miscarriage occurs, especially if it happens more than once, doctors may recommend genetic testing for both partners. This testing can help identify underlying genetic conditions that might be contributing to pregnancy loss.
Types of Genetic Testing Include:
- Karyotyping: This test analyzes the number and structure of chromosomes in both partners. It can detect chromosomal abnormalities like translocations.
- Genetic Screening: For certain genetic disorders, a simple blood test can determine if one or both partners are carriers of a condition that could affect pregnancy.
Managing Genetic Conditions During Pregnancy
In some cases, genetic counseling or treatments like preimplantation genetic diagnosis (PGD) can help couples conceive and carry a healthy pregnancy to term. PGD is often used in conjunction with in vitro fertilization (IVF) to screen embryos for genetic conditions before implantation.
10. Unexplained Miscarriages
While doctors can pinpoint a specific cause in many cases, some miscarriages remain unexplained. This can be particularly frustrating for couples trying to conceive, as they may not know what to change or how to prevent future losses.
What is an Unexplained Miscarriage?
An unexplained miscarriage occurs when all known causes, such as chromosomal abnormalities, maternal health conditions, and lifestyle factors, have been ruled out. Despite extensive testing, no definitive cause is found.
Research suggests that 10-15% of miscarriages fall into this category, where the cause remains undetermined, even after thorough investigation.
Hope for the Future
While unexplained miscarriages can be emotionally challenging, many women go on to have successful pregnancies afterward. Advances in medical technology and genetic research continue to provide new insights into unexplained miscarriages, offering hope for couples in the future.
In cases of recurrent unexplained miscarriage, doctors may recommend additional testing, fertility treatments, or even empirical treatments like hormone therapy, which can improve pregnancy outcomes in some cases.
Conclusion
Miscarriage during the first trimester is a complex and multifactorial issue, often resulting from a combination of genetic, health, and environmental factors. Many common reasons for miscarriage in the first trimester, such as chromosomal abnormalities or structural issues, are beyond an individual’s control. However, understanding these factors can help couples feel more informed and less isolated in their experience.
For those trying to conceive, focusing on improving overall health, managing chronic conditions, and minimizing lifestyle risks can be beneficial. Collaborating closely with healthcare providers, staying informed, and accessing the necessary support can help increase the likelihood of a healthy pregnancy in the future.
Each woman’s experience is unique, and while miscarriage is often devastating, it’s important to remember that many women go on to have successful pregnancies after experiencing a loss.
Read More: Should Teens Be Reading Colleen Hoover’s Books?
Is Unplugging from Social Media the Key to a Great Family Vacation?











6 thoughts on “Common Reasons for Miscarriage in First Trimester”